FAQs
Your questions about the SI joint and the SImmetry® procedure, answered.
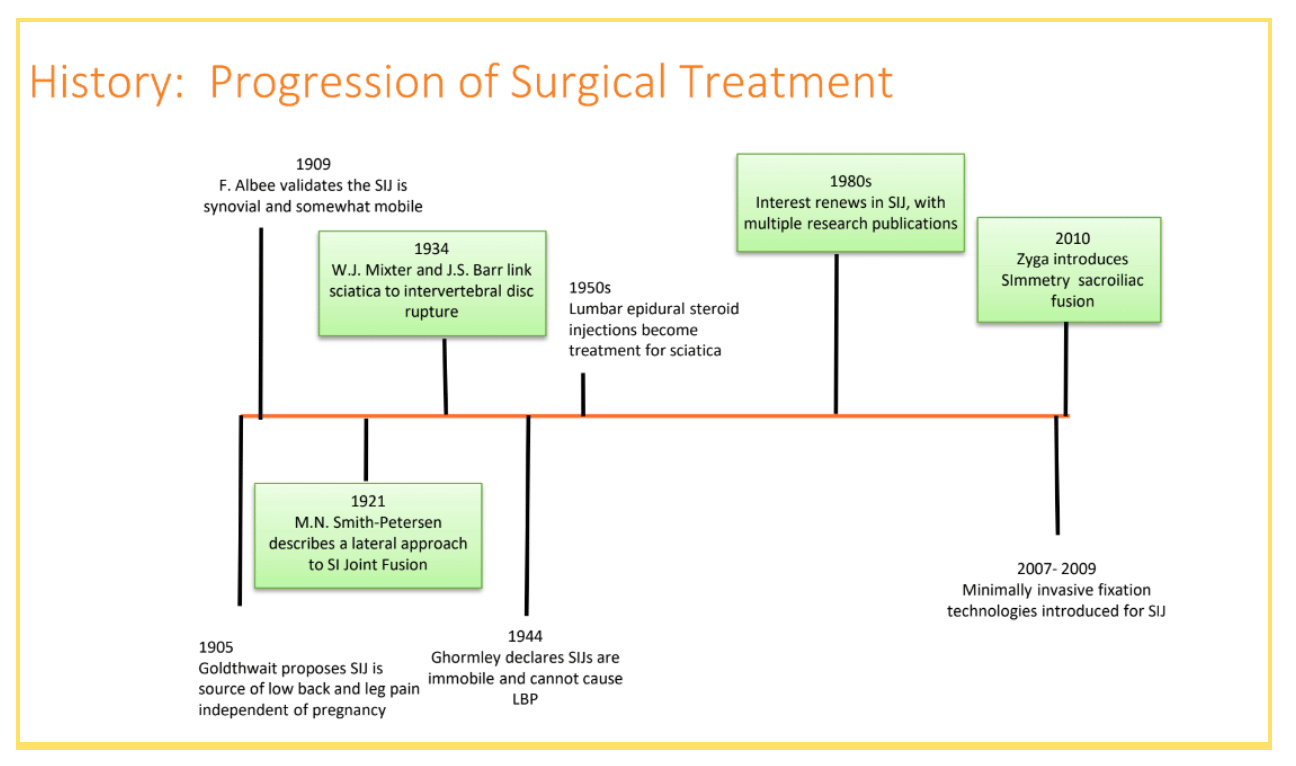
While the SI joint has been acknowledged as a source of low back pain since 1909, it wasn’t thoroughly researched until the 1980s. It then took several decades to develop surgical techniques to treat SI joint dysfunction. Because it’s so commonly misdiagnosed as a different back condition, it’s only been in the last decade or so that SI joint pain has been more widely diagnosed and treated.
Radio frequency ablation (RFA) is a process where a doctor puts a needle into the SI joint, runs a radio signal through it, and uses it to destroy the nerves in the joint.
Some people say they get relief from chiropractic care, while others don’t. Ask your doctor if they think it might help, but know that there’s not much clear data about whether or not chiropractic care relieves SI joint pain.
The SImmetry procedure was developed based on trauma literature and proven orthopedic principles to achieve a fusion of the sacroiliac joint. Fusion is the goal in most spine procedures for long term relief of pain.
New physicians are being trained on the SImmetry procedure all the time, and it’s becoming more and more widely available. Because minimally invasive sacroiliac procedures are relatively new, not all doctors have had a chance to get trained for them during their residencies. To find a SImmetry trained surgeon near you, use our surgeon locator.
Yes, the SImmetry procedure is a safe, minimally invasive procedure which uses proven orthopedic principles to provide long-lasting relief of pain. Less than 5% of patients required additional hospitalization after the procedure.
*Araghi et al; [2017] Pain and Opioid Use Outcomes Following Minimally Invasive Sacroiliac Joint Fusion with Decortication and Bone Grafting; The Evolusion Clinical Trial. The Open Orthopaedics Journal. 11. 1440-1448
Yes. In the unlikely event that removal becomes necessary, there is an implant removal instrument which can remove the screws.
About an hour, on average.
If you’re having the procedure in the hospital, you’ll usually stay 1 – 2 days. However, the procedure can also be done in an ambulatory surgery center (or ASC), where many patients will be able to go home the same day.
It depends on your individual situation – some patients need them, while others may not. Your doctor will tell you if you’ll need them so you’ll be able to get some and practice with them to get ready for recovery.
It depends on your strength and health before the surgery, but most patients only need to use crutches for 3 weeks, and some may not need to at all.
If you can manage stairs on crutches, you will be able to, but since that can be a difficult skill to learn, you may want to think about arranging your living space to minimize stair use for the first three weeks.
It depends on your strength and health before surgery. Most people will need a little help after they have surgery. You’ll need to get home, of course, and it’s good to have someone to help you while you get used to crutches. You’ll need help with tasks that involve lifting, bending, or stretching, as well as activities such as grocery shopping and cleaning, so you should plan to have someone to give you a hand for a while, even if they’re not staying with you.
It depends on the individual. There’s some pain from the incision, but many people say that pain after surgery is better than the pain before surgery. Most people use painkillers of some kind at first, but talk to your doctor about a plan that’s right for you.
Minimally invasive SI joint fusion surgery is not universally covered by insurance companies, but more and more of them are adding coverage each year. Medicare DOES cover this surgery, however. The best way to find out if your insurance covers the SImmetry procedure is call them and ask. To learn more about the insurance process, click here.
Cost will depend on your insurance coverage, deductible, and out-of-pocket maximums. However, your doctor will work with your insurance to get pre-authorization and share your costs with you ahead of time. This is an important step, so you don’t get any surprise bills. Nobody likes calling the insurance company, but make sure you get the information you need before your surgery. Visit our insurance page for more information.
Our parent company, Surgalign, does not offer a payment plan but your hospital and/or physician’s office may offer multiple payment options for any out-of-pocket responsibilities.
You may not need to worry about this code, but it may be helpful to have if you’re discussing coverage with your insurance company. In that event, the CPT code is:
27279 Arthrodesis, sacroiliac joint, percutaneous or minimally invasive (indirect visualization), with image guidance, includes obtaining bone graft when performed, and placement of transfixing device.
Remember that Surgalign has a team that might be able to help, so please give us a call (or have your doctor’s office call us) and speak to Emerson Consultants: 630.227.3809, or get in touch by email: info@surgalign.com. If, in the end, you can’t secure coverage, talk to your doctor and hospital about a price for individual payment – you may be able to get the procedure for a much lower “all-in” cost designed for people who aren’t paying with insurance.
1Surgalign Spine Technologies (2015, January -2019, August). Evolution Study Using the Zyga SImmetry Sacroiliac Joint Fusion System.
